Derrick Nelson Jr. vividly remembers the day he almost died.
Nelson was seven years old and shopping with his grandmother when she noticed that his lips had become strangely white and his skin pale. That night, he wet his bed several times, but his mother attributed it to stress, since Nelson was being picked on at school. In the morning, she gave her son milk and some food, but he immediately vomited.
“My mom called my health care provider at the time and when she told him of my symptoms he said, ‘Bring him in to the hospital—it sounds like he might have diabetes,’” Nelson says.
When they arrived at the former Michael Reese Hospital and Medical Center, Nelson’s blood glucose level was almost 800 milligrams per deciliter (mg/dl). The normal range as determined by a randomly administered blood glucose test should be less than 200 mg/dl; anything over this is diagnostic of diabetes.
Now 23, Nelson manages his type 1 diabetes with a self-adjusting insulin pump that he wears around the clock. A team of researchers led by Ali Cinar, director of the IIT Engineering Center for Diabetes Research and Education, is working to ease the burden of insulin management in patients like Nelson. They are developing a fault-tolerant, next-generation artificial pancreas (AP) system that will automatically monitor and infuse insulin according to metabolic changes that occur in response to food intake and various types of exercise, from solo fitness efforts to organized sports.
IIT, in collaboration with the University of Chicago, the University of Illinois at Chicago, and York University (Toronto), is refining such a system in a five-year study funded by two grants from the National Institutes of Health supplemented by an additional grant from the Juvenile Diabetes Research Foundation, totaling more than $5 million. The team is building upon the results of its NIH-funded earlier AP study started in 2009 that showed promising results in a small group of type 1 diabetes subjects.
“This system would revolutionize the lives of our patients...It would change their lives dramatically.” —Elizabeth Littlejohn
“We were the first group that supplemented glucose measurement information with a sports armband (BodyMedia Sensewear) that reports a person’s physiological variables, such as energy expenditure through exercise or sweating to build a multivariable AP control system,” says Cinar. “If acceleration remains unchanged but sweating increases, stress unrelated to the activity may be the culprit. That would have a different metabolic chain of events and impact on the glucose utilization than someone who is running five miles.”
Nelson and other participants in the current study spent three days under observation at the University of Chicago Clinical Research Center. For the first 24 hours, they eat meals and exercise and they regulate their own insulin. A continuous glucose monitor and the sports armband collect information on their physiological responses and blood glucose levels. For the last 36 hours, participants again go through a prescribed meal and treadmill exercise regimen attached to two continuous glucose monitors and the armband. The data collected are entered into a computer every 10 minutes and the control algorithm developed at IIT determines the necessary amount of insulin for proper body functioning. In previous trials the recommended insulin dose was assessed by the medical staff and the adjustment of the insulin pump was made upon their approval for patient safety. The adjustments will become fully automated in the new studies to make the artificial pancreas independent of medical personnel decisions.
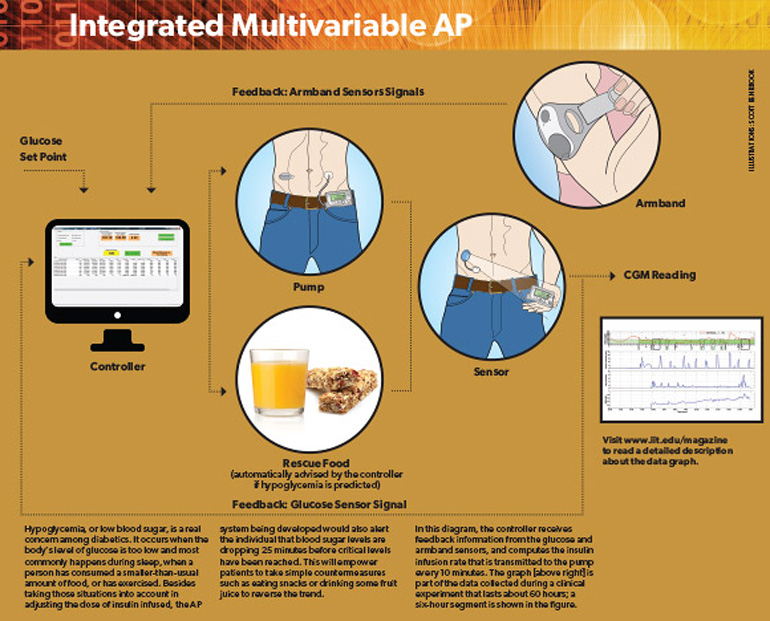
“The algorithm basically predicts going forward what the blood sugar will be in the next 30 or 40 minutes and suggests an insulin dose,” says pediatric endocrinologist Elizabeth Littlejohn, associate director of the Kovler Diabetes Center at the University of Chicago, who is responsible for the participants’ safety while they are wearing the apparatus.
“This system would revolutionize the lives of our patients,” Littlejohn says, noting that the team is working with Medtronic, the world’s largest medical technology company, to fit the algorithmic software into a device the size of a cell phone that could be worn like a pager. “They could put on the AP and go about their day; their blood sugars would be managed without the individual being involved.”
In fall 2013, the United States Food and Drug Administration approved a very basic AP developed by Medtronic that can stop insulin flow if the glucose level drops below the limit for hypoglycemia. The next generation of APs will have more sophisticated control systems that can regulate insulin infusion rates continuously to keep glucose levels within range and prevent both hyperglycemia (very high glucose levels) and hypoglycemia. While many private and university-based groups are working on this type of AP system, the IIT collaboration is the only one focusing on capturing exercise, stress, and sleep conditions automatically and using them in the controller of the AP, according to Cinar.
Nelson, who rides his bicycle year-round, is hopeful that the team’s technologically advanced AP system could one day be of long-term benefit to him as well as many of the other estimated 350 million individuals with diabetes worldwide. Although he maintains a positive attitude, the AP system would reduce the uncertainty that comes with living with diabetes.
“Living with diabetes isn’t the worst thing in the world, but it is an ongoing challenge to level everything out with my daily activities,” says Nelson. He knows that his participation in the clinical study is important. “When I first learned I had diabetes, I was depressed. But with the support of family and friends, I have a better attitude and use my diabetes as an advantage to help others.”
More Online
“Multivariable Adaptive Closed-Loop Control of an Artificial Pancreas Without Meal and Activity Announcement”: www.ncbi.nlm.nih.gov/pubmed/23544672
“Hypoglycemia Early Alarm Systems Based on Multivariable Models”: www.ncbi.nlm.nih.gov/pubmed/24187436